Video credit: Duke Clinical Research Institute Communications
In a healthcare system that often separates mind from body, a recent research study from the University of Washington School of Nursing illuminates evidence of what many have known intuitively for thousands of years – that reconnecting the mind-body divide is crucial for those struggling with addiction and chronic pain. More promising still, training practitioners and patients in this life-altering therapy is not only possible in a clinical setting, but scalable and complementary to the care that nurses already provide in a complex system where new interventions often face barriers to implementation.
University of Washington School of Nursing researchers have completed a multi-site study demonstrating significant benefits of Mindful Awareness in Body-oriented Therapy (MABT) for individuals with substance use disorders, chronic pain, and trauma histories. The research, led by Dr. Cynthia Price, shows how a simple but powerful approach of teaching people to tune into their bodies can have transformative effects on well-being.
“The research is asking whether providing people with more skills to pay attention to how they’re feeling inside is helpful for overall well-being,” explained Dr. Price, the study’s principal investigator. “We’re giving people more capacity for what is called interoceptive awareness – or awareness of internal physical and related emotional sensations through this training by teaching people how to bring mindful attention inside their bodies to know how they’re feeling.”
The multi-year study, which included sites in Seattle, Port Angeles, and Bellingham, worked with diverse participants receiving Medication for Opioid Use Disorder (MOUD) treatment. The research revealed significant improvements in pain management, reduction in PTSD symptoms, and enhanced emotional regulation. Notably, 57% of participants reported chronic pain issues, and data showed participants continued using the learned skills 9 months after completing the intervention.
“This type of work helps people engage with understanding their own personal emotional relationship to their addiction and recovery needs,” Dr. Price noted. “The MABT approach addresses a gap in services, as somatic awareness is not typically included in psychotherapy, and standard mindfulness approaches don’t teach these specific skills.”
One study participant from the mental health clinic in Harborview shared their experience from the training: “I learned how to turn my awareness inward and to be open to noticing what my body wants to tell and/or show me. I learned not only how to do this, but also the importance of implementing it in my daily life. I learned that I, my body is worthy of my attention.”
The MABT approach is particularly valuable for individuals with trauma and chronic pain histories, as they often develop coping mechanisms that involve disconnection from bodily sensations. “In the long run, this disconnection is problematic for folks,” Price explained.
“With more somatic awareness, including more awareness of the links between physical and emotional sensations, people can better engage in symptom management and feel more agency to promote well-being for themselves and in their relations with others.” – Dr. Cynthia Price, UW School of Nursing
The research has significant implications for healthcare implementation, particularly for nursing professionals. Dr. Price is currently exploring how this approach can be more broadly integrated into clinical care. “In hospital settings, nurses can bill for these kinds of services in a way that they can’t when they’re not [provided by] a nurse,” she explained, highlighting practical pathways for bringing MABT into mainstream healthcare.
The study was part of the National Institutes of Health HEAL (Helping to End Addiction Long-term) Initiative, which is working to address the opioid epidemic. HEAL has partnered with Duke University to create accessible resources that translate this research into practical tools for clinicians, patients, and other stakeholders. (The Mind-Body Partner Toolkit is available to the public.)
Dr. Price emphasized that the mindful awareness and body-oriented therapy training is firmly grounded in neuroscience. “Interoceptive processing is impaired with people experiencing chronic pain and mental health disorders. We know from neuroscience research that sensory processing is important for regulation – it’s how our [nervous] system knows how to regulate.”
With its proven effectiveness across diverse populations and growing recognition of its scientific validity, MABT represents a promising complement to existing treatments for substance use disorders, chronic pain, and trauma recovery. It is also a helpful approach for everyone, regardless of health history, to facilitate awareness and an embodied sense of self: “We all can use more skills to attend to our inner experience.”
_________________________________________
Want to know how you can support this important work? Contact sonadv@uw.edu
Interested in learning more or using mindful body awareness in your practice or personal life?
To learn more about the research findings specific to MABT, visit: Immediate Effects of Mindful Awareness in Body-Oriented Therapy as an Adjunct to Medication for Opioid Use Disorder
Recommended readings to learn more about interoception for health and well-being:
- Better in Every Sense: How the Science of Sensation can Help you Reclaim your Life by Norman Farb and Zindel Segal
- Thinking Outside the Brain by Annie Murphy
- Body Sense: The Science and Practice of Embodied Self-Awareness (Norton Series on Interpersonal Neurobiology) by Alan Fogel
- MABT Studies and Related Publications: Research – Center for Mindful Body Awareness
For health care professionals interested in MABT training opportunities: https://www.cmbaware.org/training-programs/
Other resources: UW Center for Child and Family Well-Being – https://ccfwb.uw.edu/events-classes/







 Wonkyung Jung
Wonkyung Jung


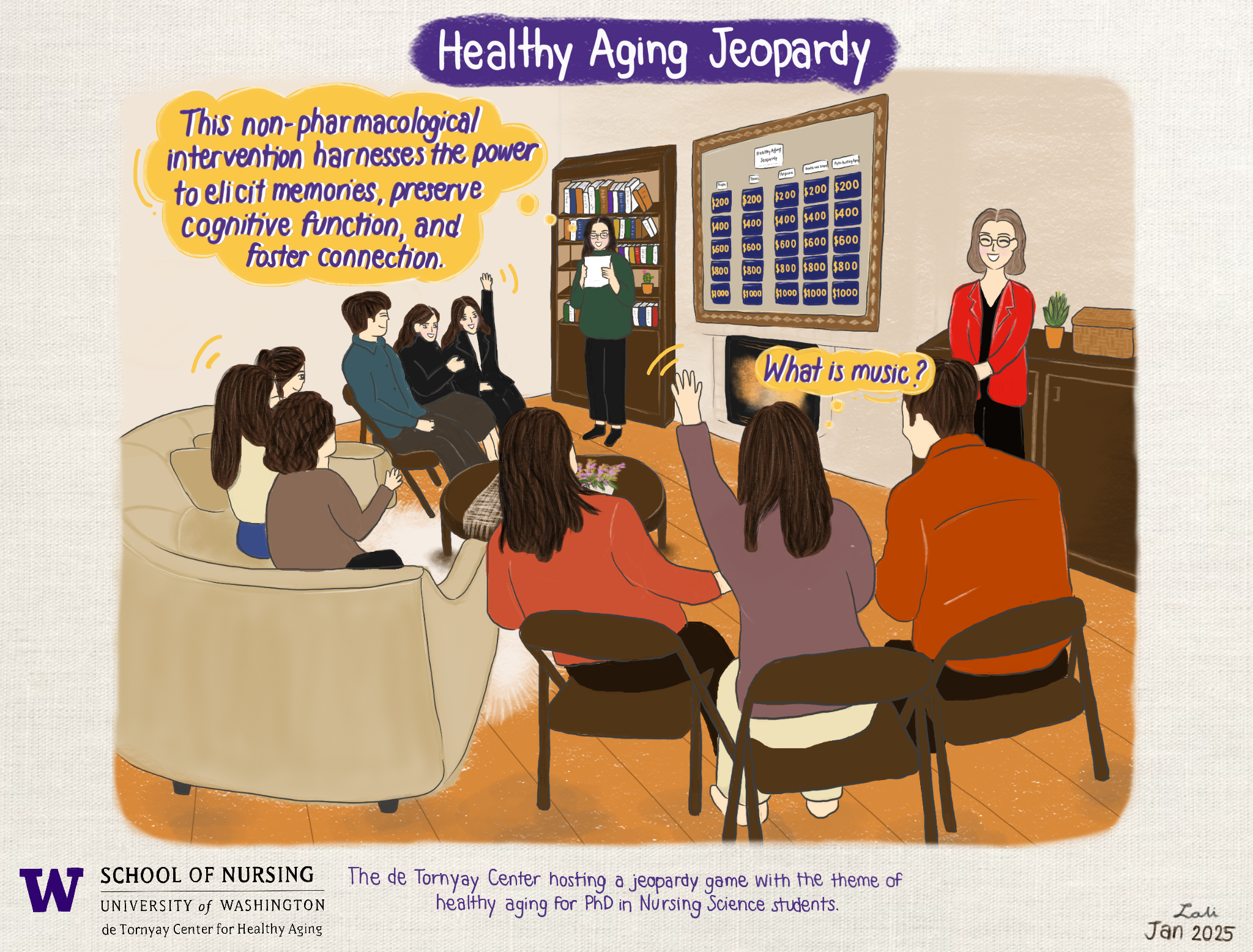
 Jeehye Jun is a postdoctoral fellow in gerontological nursing at the University of Washington School of Nursing, starting in fall 2022. She will be working with Dean Azita Emami and her research team on the project ‘Biomarker Method for Assessing the Impact of Music on Persons with Dementia and Their Caregivers’. She comes to the University of Washington after completing her PhD in Nursing Science at the University of Illinois Chicago College of Nursing.
Jeehye Jun is a postdoctoral fellow in gerontological nursing at the University of Washington School of Nursing, starting in fall 2022. She will be working with Dean Azita Emami and her research team on the project ‘Biomarker Method for Assessing the Impact of Music on Persons with Dementia and Their Caregivers’. She comes to the University of Washington after completing her PhD in Nursing Science at the University of Illinois Chicago College of Nursing.


 Olga Yudich (DNP) – Improving Coordination of Care of Highly Complex Geriatric Patients in Primary Care
Olga Yudich (DNP) – Improving Coordination of Care of Highly Complex Geriatric Patients in Primary Care Liam Malpass (DNP) – Improving Utilization of Telehealth among Clinicians Caring for Older Adults
Liam Malpass (DNP) – Improving Utilization of Telehealth among Clinicians Caring for Older Adults Boeun Kim (PhD)
Boeun Kim (PhD)